Abstract
Introduction
Rituximab and Bendamustine (BR) has been shown to be effective in the treatment of indolent non-Hodgkin's lymphomas (NHLs) with an acceptable safety profile and comparable to Rituximab, Cyclophosphamide, Doxorubicin, Vincristine and Prednisolone (R-CHOP). However, patients may develop significant cytopenias after Bendamustine exposure leading managing physicians to truncate the suggested treatment course or attenuate treatment dosages. We hypothesize that this reduced treatment intensity may negatively affect treatment outcomes.
Methods
We retrospectively analysed patients who were diagnosed with indolent non-Hodgkin lymphomas (NHL) at the Singapore General Hospital from year 2000 and received BR or R-CHOP frontline. Data was locked at 31 October 2017. Histologic diagnosis was made according to published international guidelines. The safety and efficacy of BR and RCHOP as first line treatment of indolent lymphomas was analyzed. We also evaluated if truncation of immunochemotherapy cycles or dosage attenuation impacts on progression-free survival (PFS). We define patients on BR as i) BR full - having received 6 cycles of BR at 90mg/m2/day for 2 days per cycle ii) BR attenuated - received at least 6 cycles of BR at 70mg/m2/day for 2 days per cycle iii) BR truncated - received less than 6 cycles of BR. The chi-squared and Fisher's exact two-sided tests were used for comparisons between categorical variables and the t-test was used for continuous variables. Survival probabilities were calculated using the Kaplan-Meier estimator, with log-rank analysis used to compare between different groups. All analyses were performed using Stata (Statacorp, College Station, TX, USA).
Results
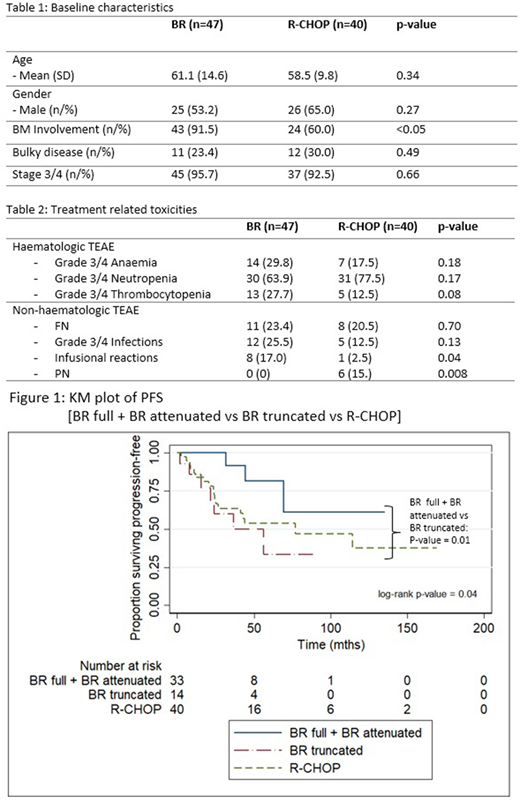
Eighty-seven patients were evaluable of whom 47 received BR and 40 received R-CHOP upfront. Amongst patients who received BR and R-CHOP respectively, histological diagnoses were: follicular lymphoma (19.2% vs 72.5%), marginal zone lymphoma (25.5% vs 7.5%), chronic lymphocytic leukaemia / small B-cell lymphocytic lymphoma (29.8% vs 5.0%), lymphoplasmacytic lymphoma (21.3% vs 7.5%), mantle cell lymphoma (2.1% vs 5.0%) and other B-cell lymphoma not classifiable (2.1% vs 2.5%). Baseline characteristics are presented in Table 1 and treatment related toxicities are presented in Table 2. There was no significant difference in treatment emergent grades 3/4 haematological adverse events between BR and R-CHOP. More patients developed infusional reactions (17.0% vs 2.5%, p =0.04) when treated with BR compared to R-CHOP. Conversely, more patients treated with R-CHOP developed peripheral neuropathy (15.0% vs 0%, p=0.008).
More patients who were treated with BR as compared to R-CHOP had treatment truncated (i.e. received less than 6 cycles) or dosages attenuated (46.8% vs 5.0%, p<0.005). The median number of cycles completed for patients who had BR treatment course truncated was 4 (interquartile range 2-4). For patients treated with BR, the reasons for treatment truncation were drug-related toxicity (17.0%), patient's decision (10.6%) and physician's decision (2.1%). 2 patients had early termination with R-CHOP treatment, 1 (2.5%) due to disease progression and another patient (2.5%) due to drug-related toxicity.
With a median follow-up of 51.0 months, median PFS for patients treated with BR was 69.5 months versus 76.9 months for patients treated with R-CHOP (p=0.26). BR truncated patients had inferior PFS compared to BR full and BR attenuated patients (Median PFS = 36.5mths vs NR, p=0.01). There was no statistically significant difference in PFS between BR full and BR attenuated patients (Median PFS = 69.5 mths vs NR, p=0.25).
Conclusion
Treatment efficacies and haematological toxicities were comparable in our patients with indolent NHLs treated with BR or R-CHOP. Despite this, more patients treated with BR had treatment truncated prematurely. The majority of such terminations were for drug-related toxicities. We found inferior PFS in patients who received less than 6 cycles of BR. Patients who completed 6 cycles of BR but had attenuated dosages did not have inferior PFS compared to patients who received 6 cycles of BR at full dose. Our findings suggest that treatment truncation with reduced treatment intensity negatively affects survival outcomes. Patients with cytopenias should be supported or have drug dosages attenuated with the aim to complete the entire treatment course for best outcomes.
Chen:Takeda: Honoraria, Other: Travel grant; Janssen: Honoraria; Celgene: Honoraria; Amgen: Membership on an entity's Board of Directors or advisory committees, Other: Travel grant, Research Funding. Goh:Novartis AG: Honoraria, Other: Non-financial support, Research Funding; Takeda: Other: Non-financial support, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal